Total Disc Replacement Surgeon in Illinois
Spine Surgery & Spine Market Overview
Anatomy and Pathology of the Neck:
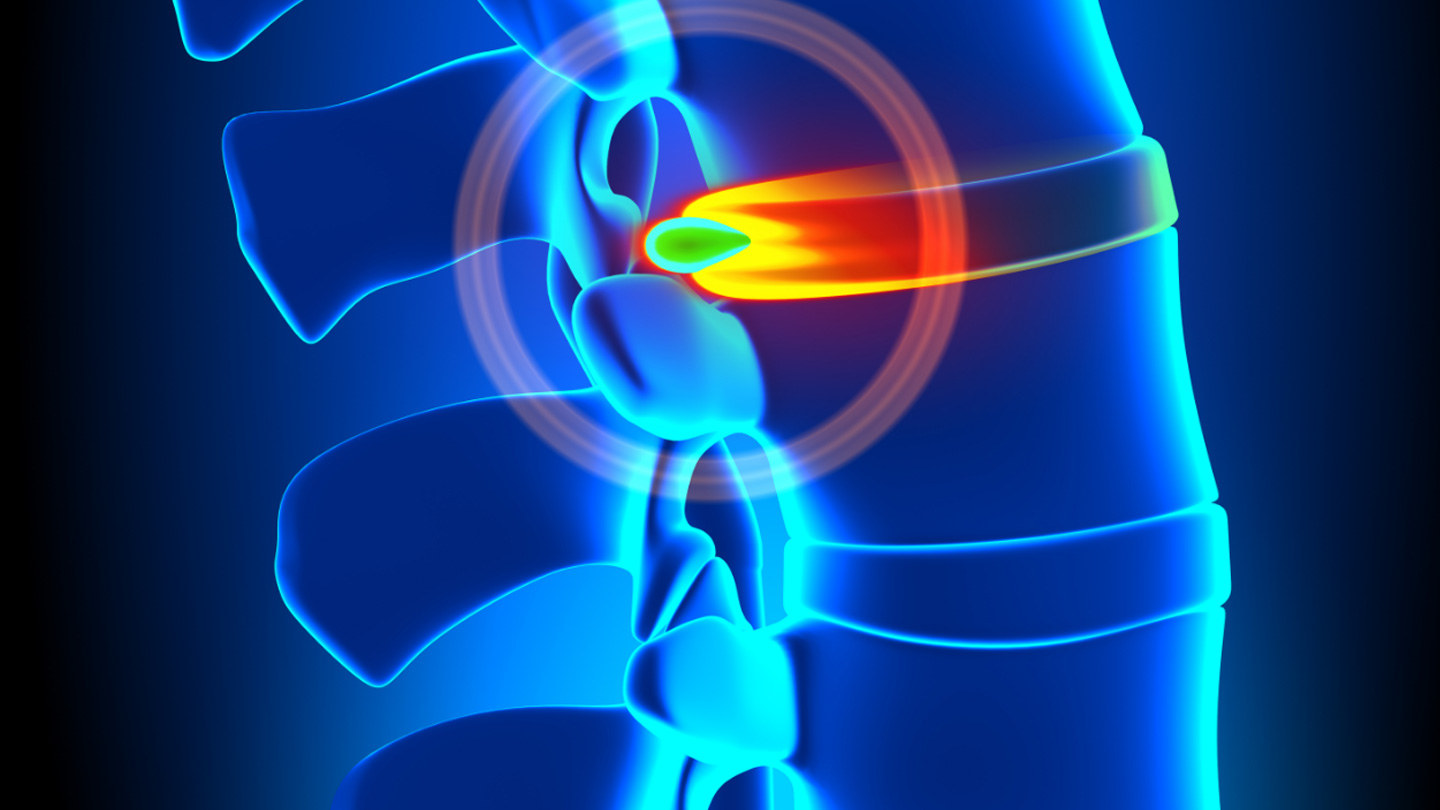
Treatment options:
Before artificial discs were available, patients would often receive an Anterior Cervical Discectomy and Fusion (ACDF) procedure to alleviate the pain from a herniated disc. In a fusion surgery, the disc is removed and either a bone spacer or a plastic implant will be placed in the disc space to restore disc height and remove pressure on the pinched nerves or spinal cord. A metal plate and screws can be placed on the front of the neck to hold the implant in place. The result of this procedure will be a segment that no longer moves, or is “fused”. The potential downside of a fusion procedure, in addition to the loss of motion, is that it can create additional stress on the spinal levels above and below it. This can cause degeneration at those levels and potentially result in another future surgery.
An artificial disc like Mobi-C is an option instead of a fusion that will also be placed inside the disc space to restore height and remove pressure on the pinched nerves. However, the Mobi-C device is designed to allow the neck to maintain normal motion and potentially prevent the adjacent levels from degenerating, possibly preventing future surgeries.
The U.S. anterior cervical spine market: (source: Global Data Market Report – 2013)
In the U.S. the prevalence of symptomatic cervical disc disease was estimated at 1.1 million people in 2012. There are over 266,000 anterior cervical procedures performed each year.
It is estimated that 30,000 of the 266,000 anterior cervical procedures in 2012 were artificial disc.
Cervical disc replacement procedures are anticipated to experience rapid growth in the near future. Growth in the next 5 years will be due to multiple factors:
- The number of FDA approved devices on the market doubled from 2012 to 2013
- A large and growing library of clinical evidence demonstrating the long term safety and efficacy of cervical disc replacement
- Expanding approved indications to include two-level cervical disc replacement (only Mobi-C)
- The demonstration of cervical disc replacement as a superior treatment to fusion for treatment at two levels (Mobi-C)
- Improved outcomes of TDR over fusion including, but not limited to, reduced re-operation rate, adjacent segment degenerations rate & surgeries, and return to work
- Expanded private insurance coverage for cervical total disc replacement
Mobi-C® Fact Sheet
The Mobi-C cervical disc is one of the most widely used cervical discs in the world. First implanted in Orleans, France in November 2004, Mobi-C has been implanted in more than 17,000 spinal levels in 25 countries.
Mobi-C entered an FDA clinical trial in 2006, in which 647 levels of Mobi-C were implanted. A total of 599 patients were involved in the clinical trial at 24 study centers across the U.S. This represents the largest clinical trial ever conducted in the U.S. for cervical disc replacement. Mobi-C received FDA approval in August of 2013, making it the first cervical disc with both one and two-level indications.
Mobi-C is made with two Cobalt Chromium alloy endplates that are plasma sprayed with Titanium and coated with hydroxyapatite, and an Ultra High Molecular Weight Polyethylene plastic insert (UHMWPE). These are proven materials that have been used in orthopedic applications for over 60 years.
Mobi-C is intended for adult patients (skeletally mature) with arm pain and/or neurological symptoms (such as weakness or numbness) with or without neck pain at one or two adjacent levels from C3 – C7 in the cervical spine. Patients should have failed non-surgical care (such as physical therapy or medications) for at least 6 weeks, or shown signs of progressively worsening symptoms. Disc damage needs to be confirmed by a doctor’s review of CT, MRI, or x-ray images. A doctor should always be consulted for proper indications and use of Mobi-C.
Mobi-C – How it Works
Mobile Core
- Mobi-C is designed to replicate the natural motion of the cervical spine.
- Mobi-C contains patented Mobile Core Technology™ that allows the polyethylene core to slide and rotate inside the disc for self-adjustment to the cervical spine movements. This means that Mobi-C
can react to the normal motion in the cervical spine. - In addition, the mobile core is designed to reduce the stresses between the implant and adjacent bone, eliminating the more invasive fixation features found in other cervical disc replacement devices.
- Mobi-C provides bone sparing fixation without chisel cuts into the small vertebral bodies of the cervical spine. Competitor’s discs achieve their fixation by drilling keel cuts or screw holes into the bone,
which can prevent safe implantation at two levels. - Mobi-C was designed without a keel and therefore to be specifically applicable for both one and two-level indications.
Mobi-C – Clinical Trial Results, 24 month Primary Endpoint
- Overall trial success was 69.7% for Mobi-C and 37.4% for fusion, which represents statistical superiority (p< 0.0001).
- The rate of secondary surgeries at the operated level for Mobi-C was 3.1% versus 11.4% for fusion.
- The percentage of subjects who demonstrated adjacent segment degeneration (determined by x-ray) was:
- 2.9% of Mobi-C patients compared to 18.1% of ACDF patients at the inferior adjacent level
- 13.1% of Mobi-C patients compared to 33.3% of ACDF patients at the superior adjacent level
- Mean return to work time was 20.9 days shorter for Mobi-C patients compared to fusion patients.
- 78.2% of Mobi-C patients showed improvement in Neck Disability Index (NDI) based on the FDA success criteria versus 61.8% of fusion patients.
For detailed clinical results, see the Mobi-C Summary of Safety and Effectiveness document (SSED) online at www.ldr.com or www.fda.gov or visit www.cervicaldisc.com
Request an Appointment